Tilt Table Test for Children
What is a tilt table test for children?
The tilt table test is done to find the cause of fainting (syncope). Syncope is a brief loss of consciousness and muscle tone (or posture) when not enough blood gets to the brain. In children, fainting is usually harmless. But in some children, fainting can be serious. This is often because of a heart problem or sometimes a neurological problem. Tilt table testing is done with a special table or bed that changes a child's position from lying to standing. The child's blood pressure and heart rate are checked while the child is in the different positions.
Why might my child need a tilt table test?
If your child has episodes of fainting, their healthcare provider may advise a tilt table test. Syncope can have many different causes. It may happen only rarely or it can happen often. Some causes of syncope may include:
-
Vasovagal syndrome (or neurocardiogenic/reflex syncope). A sudden drop in blood pressure occurs with or without a decrease in heart rate. It is caused by an exaggerated but normal nerve response to some triggering event that can affect the heart and blood vessels. This is the most common cause of syncope. It can follow periods of extreme emotion. It is generally a benign condition. A tilt table test is most commonly done to confirm this condition if it's suspected.
-
Arrhythmia. The heart rate is too slow, too fast, or too irregular to keep enough blood flowing to the body, including the brain. This is a rare, but potentially dangerous cause of syncope.
-
Structural heart disease (muscle or valve defects). There may be problems with the heart muscle or one or more of the heart valves. This may cause a decrease of blood flow to the body, including the brain. Inflammation of the heart muscle (myocarditis) may also cause fainting. The heart muscle becomes weak and isn't able to pump as well as normal. The body reacts to decreased blood flow to the brain by fainting.
-
Orthostatic hypotension. This is a drop in blood pressure that occurs when a person has been standing for a while or changes when a person goes from a sitting to a standing position. Blood pools in the legs, preventing a normal amount of blood from being pumped to the brain. This brief drop in blood flow to the brain causes a person to faint. This is more common in older adults.
Other problems that can cause or imitate syncope include:
-
Head injury
-
Seizure
-
Stroke
-
Inner ear problems
-
Dehydration
-
Low blood sugar
-
Breath holding episodes (typically in younger children between ages 6 months and 2 years)
-
Anemia
-
Mass or tumor in the brain
-
Aneurysm or abnormality of a blood vessel in the brain
-
Urination or having a bowel movement
-
Coughing
When a healthcare provider sees a child with fainting episodes, they'll carefully check the child's medical history and do a physical exam. Tests include an electrocardiogram (ECG) and often an ultrasound exam of the heart (echocardiogram). If the exam or history doesn't reveal a cause for the fainting, and the child has no history of a heart condition, then further tests, such as a tilt table test, may be done.
What are the risks of a tilt table test for a child?
The primary risk for your child during a tilt table test is fainting. If fainting does occur, your child is in a safe, supervised setting and won't be hurt.
How do I get my child ready for a tilt table test?
Your child shouldn't eat or drink for a certain amount of time before the test. Talk with your child's healthcare provider about the specific amount of time.
What happens during a tilt table test for a child?
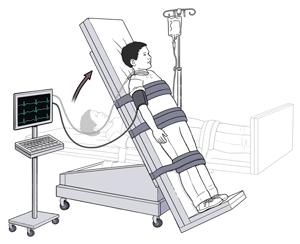
A tilt table test may be done in a special clinic or in the hospital. It may last from 30 to 90 minutes. The test has 2 parts as follows:
Part 1
-
Your child will lie on a special table or bed. Straps will be placed across their chest and knees to help them stay in the correct position.
-
A healthcare provider may put an IV (intravenous) line in one of your child's arm veins to give medicine.
-
The provider will put a blood pressure cuff on one of your child's arms to check blood pressure throughout the test.
-
The provider will attach electrodes with wires to your child's chest. The wires are attached to an ECG machine that lets the provider keep track of your child's heart rhythm throughout the test.
-
The provider will tilt the table so that your child's head is higher than their body. Your child will stay in that position for several minutes. The provider will watch for changes in your child's blood pressure and heart rhythm. The provider will also watch your child for dizziness, fainting, and other symptoms.
-
The provider may raise the table even higher or repeat this part of the test while watching for changes in your child's blood pressure and heart rhythm.
-
If your child's blood pressure drops or if syncope is reproduced, the healthcare provider will end the test and promptly have the table placed in a flat position.
Part 2
-
If there are no changes in blood pressure, the provider may decide to give your child medicine through the IV line. Isoproterenol or nitroglycerin are the two most commonly used medicines. They may either cause your child's heart to beat faster and harder or cause the blood pressure to go lower. This makes your child more sensitive to the changes in positions.
-
The healthcare provider will tilt the table so that your child's head is raised. They'll watch for changes in your child's blood pressure and heart rhythm.
-
The provider will stop the test and the medicine and place the table in the flat position if your child's blood pressure drops. If it doesn't drop, the provider will end the test after watching your child's blood pressure and heart rhythm for a while.
What happens after a tilt table test for a child?
Your child may feel tired and nauseated for a while after the test. They'll be watched for about 30 to 60 minutes. You provider may give you specific instructions. Test results may be available right away or in a few days.
The test may not cause any symptoms or changes in your child's ECG or blood pressure. If so, your child may need more tests or procedures to find the cause of the syncope.
Next steps
Before you agree to the test or procedure for your child, make sure you know:
-
The name of the test or procedure
-
The reason your child is having the test or procedure
-
What results to expect and what they mean
-
The risks and benefits of the test or procedure
-
When and where your child is to have the test or procedure
-
Who will do the procedure and what that person’s qualifications are
-
What would happen if your child didn't have the test or procedure
-
Any alternative tests or procedures to think about
-
When and how you'll get the results
-
Who to call after the test or procedure if you have questions or your child has problems
-
How much you'll have to pay for the test or procedure